Originally published on Counselling Directory in three parts
It has been said that if you have met one autistic person, you have met one autistic person (Dr Stephen Shore)
Note: If you fill in this worksheet, consider who you might share it with and why. Some of the questions will contain a lot of confidential information about your health, history, and how you process the world. I hope it will help you understand more how autism uniquely affects you, and to explain parts of this to people who know you professionally or socially, but your safety and confidentiality both need to be considered before you share your answers and choose which ones to share and with whom.
Disclaimer: Autism affects each person uniquely and you may not align with every aspect of this worksheet.
Autism Spectrum Condition (henceforth Autism or ASC – I avoid the term ‘Autism Spectrum Disorder (ASD)’, as I do not feel it a disorder, but a neurodivergence within a neurotypical world) affects everyone uniquely, and although there are common challenges a person on this spectrum may face, the way they are expressed will be unique for autistic person. This article seeks to go through some of the ways autism may be expressed so you can talk about how your autism uniquely affects you.
As with many diagnoses, we can conceptualise what ASC means for an individual or for ourselves, but it will be uniquely expressed in every individual, and going through this worksheet will enable you to consider how ASC is uniquely expressed for you. I have written this especially considering if you are starting therapy, but this could also be used to explain your autism to other professionals or people who might be interested.
This article is a brief introduction to how autism affects individuals. I highly recommend checking out the National Autistic Society for more specific articles on these topics or searching through Counselling Directory’s articles for more detailed articles.
You can also download this article as a worksheet that just has the headers and some prompts on how to answer how these things affect you. I do not have ASC but have consulted in writing this and am very open to feedback on if this is useful as a tool or how it might be used/adapted.
1. Diagnosis
Have you got a formal diagnosis of autism? It may be that you identify with some traits and are wondering if you do, or that you self-diagnose. If you’re younger than 40, you may have been diagnosed whilst you were at school by an autism team, but sometimes autism can be masked by other traits, or you can mask (perform socially to hide autism) and it may not have been noticed. Autism is a way of processing the world around us and to be diagnosed with ASC you would need to fit the criteria since the age of three.
It’s worth considering the pros and cons of seeking and getting a diagnosis. Victoria Hughes’s talk on YouTube expands on some things to consider. To briefly summarise: getting a diagnosis can be a huge relief for some people after years of feeling different or self-blame; it can provide a diagnosis that we can also use to explain to others, it opens some options for support, and it can provide some validity and recognition of our individual support needs. It can also have some implications in terms of stigma which can be attached to a diagnosis; a diagnosis is a lot to process as ASC is a lifelong condition, and the process of getting a diagnosis itself can be costly privately or with lengthy waiting lists.
Whether you have a formal diagnosis or not, different parts of this worksheet will affect you, and it can still be useful to reflect on our needs to explain it to others and support ourselves.
2. Learning Difficulties
Mencap is a charity working with people with learning difficulties (LDs), and a great resource for more information and support around LDs. They mention that around half of autistic people also have an LD. LDs can be classified from mild to severe. With an LD you may need support with your care needs, communication, and in learning new information.
More severe LDs can be more noticeable. A term is sometimes mentioned called ‘high functioning’ autism for an IQ above 70. This term is going out of fashion because it implies that someone without an LD doesn’t need support, whereas any diagnosis of autism is recognised under the Equality Act (2010) and deserves an assessment for support to thrive in a neurotypical (NT) world. You also likely found that your communication and learning developed at a different pace to peers in school, and you needed to find your own way to process and learn.
3. Other Neurodivergences
Autistic people are more likely to have other neurodivergences alongside their ASC. This includes ADHD, dyslexia, OCD, dyspraxia, and others. Some of those conditions can mask autism or vice versa (e.g. both autism and OCD can involve a sense of peace or joy from repetition and order, whereas ADHD might mask autism in a child). You are a whole person and each part of you interacts, so it is worth considering how other diagnoses of neurodivergence affects you individually, as well as how that might interact with your ASC.
This article doesn’t go into much detail about other neurodivergences; The National Autistic Society is a good resource for articles, as is Counselling Directory, and the ADHD Foundation.
4. Social Communication
Social communication concerns how we communicate with others. It concerns the language we use, phrases we repeat, our prosody (tone, intonation, pace of words), body language, and whether we use aids to communicate.
4.1. Communication Preferences
Language development can be delayed for autistic people. Some people may not communicate verbally or have limited verbal communication styles. Communication styles may also change, for example with selective mutism where a person is unable to speak in certain high-stress situations. Some people may communicate verbally, whereas others may prefer gestures or visual aids.
Language aids: Makaton is a form of simplified sign language done alongside verbal communication to aid communication. This YouTube Channel teaches some words in Makaton or SingingHandsUK sign songs in Makaton.
Picture Exchange Communication Systems (PECS) allows a person with limited or no verbal communication to exchange pictures of items they would like or their needs, in order to build up sentences and communicate.
It may be that you use other aids or enhancements to clarify your communication.
Not being understood when we try to communicate, or being unable to express when something is an issue for us, can be a huge source of frustration to individuals.
4.2. Auditory Processing
We have discussed how some people do not communicate verbally or need assistance/aids to do so. Likewise, there may be preferences in the form of communication you receive. Have you, for example, ever had a phone call from a friend or relative and felt an intrusive dread at the thought of being thrust into a conversation with them? An unexpected phone call can lead to a lack of control or routine and be seen as quite threatening.
We can be guilty, when we communicate with someone, of assuming our communication preference is the same as theirs when they may feel much more settled and safer with a different form of communication. Synchronous (real-time) modes of communication such as phone calls, face-to-face meetings and video messaging, carry the intricacies of non-verbal communication and may not provide people the processing time they need to reply. Asynchronous (non-instant) communication styles such as text, email, chat forums, or letters, can often provide the space to reflect or time to respond when a person feels safe and clear.
Face-to-face meetings will also involve a lot of other sensory and facial stimulation that could be overwhelming and block safe reflective communication. Since the pandemic, apps like Zoom have become commonplace in the therapy world. There are increasingly more mediums to choose from such as Discord, which can be used whilst interacting within your favourite video game. What method of communication provides you with the optimal level of emotional arousal where you can communicate safely and be heard? This may be, for example, video messenger, text, calls, face-to-face meetings, or something else.
4.3. non-literal communication
I am aware that my language can use sayings or metaphors that allow me to add emphasis or create a visual connection in imagining a metaphor (for example in section two, I said ‘going out of fashion’ and I didn’t mean that it was cool and fashionable to say “high functioning”, I meant that the term is more historic).
This can be confusing though – for example, why would we say “break a leg” before a performance when we mean “I hope it goes well”? For some autistic people, it can be difficult to know what people mean when they use sarcasm/irony (‘beautiful day’ when it’s raining), exaggerative language (‘I was in traffic for hours this morning’ when we mean it was busy), or banter. This can create a difficulty in following conversation when abstract terms are used.
An autistic person may communicate with very clear sensical language but may struggle more with the prosody that others use in their speech such as the tone or intonation when we mean a question, or the flow of pace that changes as we add emphasis to words. This can be another reason why asynchronous forms of communication can be more comfortable and allow more clarity of meaning.
Some autistic people (particularly children as a method to learn language) may also do something called echolalia, repeating phrases they have heard repetitively. The echolalia may sound strange or out of place, and the intention behind it may be to communicate or to self-soothe and not communicate. It can also be considered “copying to cope” – a way to practice social etiquette and fit in by repeating what others say. It may be immediately after hearing something said, or a delayed repetition of words that someone has said, or they have perhaps heard elsewhere for example in a favourite show.
The rise of memes, GIFs, and emojis has provided a rich means of online communication where we can repeat the essence of the meaning with an image that seems out of place; in the same way that there may be rich communication behind echolalia.
5. Social Interaction
Social interaction is how we can use our communication to interact socially with others, and how we can interpret their communication back. We have outlined how a person with ASC may have difficulties communicating with others or interpreting some of the subtleties of their communication which can make interacting socially difficult.
5.1. Social Etiquette
Social interaction has lots of subtle rules that are unspoken or shift mysteriously and are somehow sensed by neurotypical people. This can create a lot of social anxiety to somehow belong and follow these rules and there can be a strong sense of ‘getting it wrong’ in a neurotypical world yet not knowing why or if they are wrong.
An example of this, which a neurotypical person might relate to, is when you go abroad on holiday when showing the soles of your feet, wearing shorts, or shaking with your left hand could cause immense offence, and you might be completely unaware as to why because you are unaware of the cultural context. The same can be experienced by an autistic person when social etiquette is unspoken yet there is a neurotypical expectation for it to be understood. An autistic person may also inadvertently communicate non-verbally and not understand why others misinterpret them.
Social etiquette changes in different environments (for example speech volume in the library, cinema, football field, or a restaurant), between people (for example with personal space; a comfortable distance between people will be different if they are within our family, our sexual partner, a friend, colleague, or stranger), and even with the same person (is it appropriate to talk about my special interest now, or is this person not interested?) and yet most neurotypical people seem to somehow know these unwritten social rules.
5.2. Reading Others
We mentioned that autistic people may struggle to understand others’ non-verbal communication. When we interact with others we use body language, distance, prosody, imagery, sayings, and communicate our feelings within our speech; within a group, communication is even more complex with roles/positions/hierarchy, processing space, and dynamic relationships playing out. When we speak, there are motives for speaking and intentions behind the message, but that intention might not always be communicated. An autistic person may struggle to interpret the entirety of communication and, because of that, struggle with the interaction.
There is a myth that autistic people don’t have empathy or theory of mind – it’s more that they may struggle to read all the non-verbal communication cues and have some rigid expectations that work for them and can cause distress when deviated from. The same can also be said about some autists’ ability to communicate non-verbally. They may be presumed rude or insincere if their facial expressions do not match the tone of what they are communicating (e.g. if they are frowning because of pain that they may not detect due to interoceptive issues, that could come across as if they are angry at someone), as insincere or robotic if their tone and pace lack the expected prosody of an interaction, or as invasive if our proprioceptive needs mean we stand too close to someone than is ‘expected’.
Honesty and congruence in communication can also be a beautiful neurodiverse trait, that neurotypical people are less used to with an expectation of there being more communicated than is actually being said leading to a sense of suspicion.
5.3. Eye contact and Physical touch
5.3.1. Eye Contact
Autistic people are likely to experience sensory processing issues. Eye contact carries a lot of sensory information, and a lot is communicated within the micro-expressions on the face. For this reason, direct eye contact can feel overwhelming and deeply intrusive, and many autistic people will feel safer and more able to process if they are free to not stare at a person.
Neurotypical (NT) people will glance often at the face and eyes of the other person during conversation, holding it for a second or two, but likely empathise that just staring into someone’s eyes is intense (often either romantic or if we are going to fight) – for an autistic person this can be more extreme and permission to not hold a gaze can help them be more attuned to conversation.
5.3.2. Physical Touch
I will cover sensory processing later, but physical touch such as hugging, handshaking, pats on the back, or contact in sports can feel deeply intrusive and create a sense of overwhelm. Again, an environment may be more comfortable for an autistic person if they know that they are not going to be touched, or if explicit consent is gathered before something like a handshake.
6. Social Imagination
This is the third and final part of the traditional ways of looking at Wing and Gould’s “Triad of Impairment model”. Social imagination means the tendency to enjoy repetitive behaviour, to invest in special interests, and to struggle when structures we are familiar with change. To an autistic person, the world can appear incredibly chaotic and difficult to understand, and structure provides some comfort that comes from the anxieties of being in a NT world.
6.1 Structure, Change and Routine
The world can feel very out of control, just as social situations can feel chaotic and unpredictable. Having a routine can help an autistic person feel settled and alleviate anxiety. This might involve a timetable or board of what is happening in the day, having a routine of what meals are eaten on certain days, or ritualising tasks such as the order we shower our body parts. Any measures we can take to predict the uncertainty of the world can create a sense of safety. This may, for example, mean planning a new bus route or being aware of interruptions that might happen at a concert to prepare for them.
One tool to support someone is understanding and creating a sense of understanding of tasks or new situations involves using social stories, a comic book-like explanation of a task that breaks it down into smaller consequential pieces.
We need to understand these routines, repetitions, and rituals as coping mechanisms for anxiety and intolerance towards uncertainty. An autistic person may find themselves incredibly dysregulated and distressed if the routine is broken or the ritual amended (e.g. the supermarket doesn’t have the right food, the normal route has roadworks, or an event is cancelled). Transitions in life (new role, going to university, a bereavement, a new relationship) can also be distressing due to added unpredictability.
6.2 Repetetive Behaviour and Stimming
Stimming is a repetitive behaviour that an autistic person will use to comfort themselves and self-regulate. Sometimes we stim to regulate sensory sensitivities for example if our balance is under-stimulated, we may rock back and forth, or if we struggle to connect with our limbs then ‘hand flapping’ might regulate that sense.
Stimming can also provide a point of focus if experiencing sensory or emotional overwhelm, for example humming in a restaurant can block out other background noise just like monks might chant ‘Om’ when meditating. Stimming creates an association of peace or regulation and can feel incredibly pleasurable to do. If you Google ‘Fidget Toy’ or ‘Stimming Toys’, you’ll find a wealth of items that can help regulate.
The important thing is to consider what need stimming is meeting, and how that need can be met to regulate the person in a way that they can most fit into a social setting without unwanted attention. Some people’s stims can put them at risk (e.g. head banging or biting) – can we work out how it is regulating the person, and if the regulation from that stim can be replaced to keep them safe (e.g. a helmet if headbanging, or hard sweets to bite).
Forcing someone not to stim can be torturous because we are taking away a coping strategy that they are using to self-regulate without providing an alternative way of self-regulating.
6.3 Time Keeping
Time is a construct that helps us synchronise with others and order our days. It can help with that sense of ordering a chaotic world. An autistic person may find being punctual and ordered with time helps create a sense of safety. Some of our language can be non-literal (e.g. “I’ll be five minutes” when we mean “I am close to arriving”) or we can use words related to time that are abstract (“we’ll be there in a while or later today”).
Speaking in a quantifiable way in terms of time can be clearer, and sticking to time boundaries can help add to that sense of safety. In therapy, for example, the session may start at 5pm and last one hour – this provides a predictable structure that could cause distress if it regularly over/underruns or starts late.
6.4 Special Interests
Autistic people usually have several special interests (SI). These are areas, hobbies, or things that the person is particularly interested in. Some examples might be trains, mice, computing, anime, roleplaying games, Egyptian history, and stamps. A person’s SIs may also change throughout life. SIs are different to hobbies or passions a neurotypical person might have but of a similar flavour.
An autistic person will derive a rare sense of true pleasure and an ability to hyper-focus on the special interest; it provides a sense of mastery, which may even lead towards a fulfilling career (note, a significant proportion of autistic people face unemployment – it is a protected characteristic under the Equality Act (2010) and there is a lot of support towards employment).
An SI can also be a great way to build community – especially with groups and forums online. SIs can also be detrimental; it may be that in deriving so much pleasure from it, the person struggles to not steer conversation towards their SI (a topic they are very much comfortable and in control of), and they may also struggle to focus on other areas of their lives that are easy to neglect in order to focus on the SI.
Films like “Rain Man” (1988), or the show, “The Good Doctor”, present autistic people with Savant condition where they have incredible skill in an area from their SI and high intelligence. This is said to affect around 10% of autistic people and it is a myth that “you have autism so you must be really clever and good at X” which represents some but not every person.
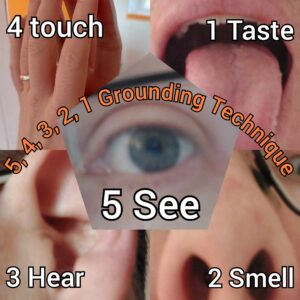
7. Sensory Processing Disorder (SPD)
SPD means that you are either hyper (over) or hypo (under) sensitive to stimuli from the different senses. A person may experience both hyper and hyposensitivity at different times and differently in different senses, and with that will either find themselves overwhelmed by too much sensory information or feel under-stimulated and seek out sensory stimulation to feel regulated.
Spectrum News quote SPD as affecting 15% of the population, but 90% of autistic children. A sensory profile is unique to everyone in how they go about seeking equilibrium to regulate. Stress and the environment also play a part if multiple senses are being stimulated.
Sensory overload is when there is too much information to handle – if a neurotypical (NT) person stood next to a speaker at a gig, it may be too loud so they move away, or if the stage light flashed in their eyes, they might close them or relocate. A person with SPD may find that they cannot escape the light or noise and experience overwhelm, which can be a major reason for behaviours that challenge (‘meltdowns’). If we can seek to understand our sensory profile, we can find ways to regulate ourselves to an optimal level of stimulation and plan for environments that might be likely to lead to overwhelm.
People without SPD are also better able to filter out background information (e.g. writing this in my living room, I can hear the clock tick, smell my brewed coffee, notice the red TV standby light, and feel the weight of my hoodie – all of which I mostly filter out), whereas if we have processing hyper-sensitivities, the stimuli from those background senses can be too intense to ignore.
7.1. Physical Touch
Touch is a series of different senses in the skin but also other body parts such as the tongue, genitals, and epithelial cells. With touch, we detect pressure, pain, heat, and texture. A person with hyper-touch is likely to feel overwhelmed by physical touch such as being pulled in sports or hugged; they may find that clothing rubs and is uncomfortable, chairs and bedding feel too hard, or a sense of disgust at certain touches like in bathing. Touch sensitivities can even be experienced as allodynia, where gentle touch can physically be experienced as pain – especially if the person is already overwhelmed.
A person with hypo-touch might appreciate weighted blankets, being squeezed, or tough play like in rugby; they likely enjoy hard food like nuts and feel regulated when touch is firmer and more pronounced.
7.2. Taste
Taste is a combination between smells and the different taste receptors on our tongue and mouth. A person who has hyper-taste will likely find many foods are too pungent, strong, or the texture off-putting. They may experience an avoidant or restrictive diet (ARFID) where only certain foods don’t create a sense of sensory overwhelm or a feeling of sickness which can cause significant anxiety when their diet is changed, or if eating out. Fruit and vegetables, for example, are variable in how they taste depending on ripeness and between batches such that two apples from the same tree could taste very different and be hard to predict.
Hyper-taste will also likely cause intolerance to herbs and spices that others may not notice. It can also combine with other senses such as hyper touch where food that is too chewy or mushy may create a sense of disgust because of the mouthfeel of the food’s texture, even leading to gagging. A person with hyper-taste isn’t a ‘picky eater’ or difficult, it’s that too much flavour creates a sense of disgust and sensory overwhelm that prevents the person from being able to eat (just as I might feel revulsion at trying to eat a very strong curry, or a pregnancy may create sickness at eating certain foods).
Someone with hypo-taste may need to add more spices and flavourings to food to enjoy it and feel regulated. They may be keen to try lots of dishes, and even try eating objects (Pica). It could combine with touch to want foods with interesting and varied textures.
7.3. Smell
Smell impacts much of taste, but also on our tolerance and detection of aromas. A person with hyper-smell may find they are sickened and unable to eat if there are strong aromas in a room (for example, boiling cabbage), or that some foods have a smell that creates revulsion. They may also be sensitive to smells like perfumes, candles, cleaning products, animal smells, flavoured laundry detergent, or if a toilet has been unflushed such that they need to leave the room in the presence of these smells and may find themselves coughing or overwhelmed by it (just like you might be if someone has really overdone it on aerosol deodorant). Smell sensitivities can be difficult to risk assess for and prepare for (e.g., ear plugs work with sounds, but it’s harder to plug a nose) in environments outside of the home and can make that environment intolerable to be in.
Hypo-smell means needing stronger smells to feel regulated due to a less sensitive nose. A person may appreciate olfactory stimulation exercises such as fragranced jars to smell, use more spices in their cooking, and more potent perfumes or fragrances in their home. A person with hypo-smell may also not notice if they have body odour issues or notice smells people may find repulsive such as rot, faeces, or the smell of gas leakages. This can lead to a risk of bullying if there are body odour issues and the need for schedules to remember to wash if we are sweaty, or a risk of danger from not noticing smells that usually warn us.
7.4 Vision
Vision relates to the brightness of lights, colour preferences – with some colours being overwhelming and others calming – and noticing motion in the background such as registering other people in a crowded room or the flickering of fairy lights on an Xmas tree.
Someone who is hyper-visual may find the world to be too bright outside and find themselves overwhelmed or fatigued by the sun or bright lights – possibly appreciating sunglasses to dampen it down. They may also find certain colours too stimulating and others less or more tolerable. With food, they may prefer blander-coloured foods such as white bread or porridge rather than brightly coloured foods. They may also find that they notice the flashing light of a charging phone or the movement on a TV screen in a pub that they are unable to ignore.
Someone who is hypo-visual will likely appreciate more vibrant bright colours, bright lights, and lots of visual sensory information going on around them such as a crowded club to feel regulated. They may be in danger, for example, of not noticing cars when crossing the road. They may also find darkened rooms at bedtime too bland to feel regulated and safe enough to sleep, perhaps often using the phone before bed.
7.5. Auditory
Auditory relates to the sounds we hear within and outside of us, as well as our ability to filter background noise. Someone who has hyper-sound may notice their own internal body noises such as their heart beating and struggle to ignore it, they will also likely notice background noises such as the humming of electrical devices or a clock ticking and need a space of quietness to feel regulated or to sleep. They will likely find performances (such as concerts, the cinema, or firework displays) have the volume up too loud and experience overwhelm at the noise. A person with hyper-sound is likely to notice background conversation if in a crowded place like a restaurant and struggle to focus on the conversations in front of them. They may carry earplugs with them if they begin to experience overwhelm or the volume is too loud and need to leave the environment.
Hypo-sound will leave a person feeling as though things aren’t loud enough; they will likely turn up the volume on their devices and may also talk loudly as normal talking volume isn’t regulating. They may also not notice background noises and have a similar risk of danger from not noticing cars.
Both hypo and hyper-sound may find making a noise regulating if they are experiencing overwhelm as it creates one central sound to focus on (hyper) or gives a volume that is comfortable (hypo).
7.6. Proprioception
Proprioception is the spatial awareness of our limbs in relation to our body such as our hands and feet. It controls fine motor control such as the force and pressure we need to stroke a cat without it being uncomfortable or learning to write. It controls our strength or awareness of our strength and posture as well as awareness of how much our joints can extend without hyperextension or risk of injury. It also involves awareness of our body in relation to other things and people.
A person with hyper or hypo proprioception may be called clumsy “you don’t know your own strength” – often spilling or walking into things. Fine motor skills like playing an instrument may be challenging; they may also find that they misjudge personal space or are unaware of how close they are to a person. They may find they have joint issues from hyperextension. A person with hypo-proprioception may need to stomp, jump, and do lots of physical activity to feel regulated; tools such as weighted armbands may be used on the limbs to help create awareness of their location in space.
7.7. Vestibular
The vestibular system is within the inner ear and is used to detect balance. A person with hypo-vestibular may rock back and forth or spin to feel regulated and appreciate physical activities involving motion. A person with hyper-vestibular may find they feel dizzy with course movements or if their feet are off the ground and may experience car sickness. The vestibular system can also affect learning to walk or do new physical movements or balancing.
7.8. Pain
Pain helps us to be aware when our body is injured so we can treat that body part or avoid further injuring it. Pain can be from damage, but also from heat or cold such as when we are drinking a boiling cup of tea. Someone with hyper-pain may struggle to ignore aches or pains they suffer or to cope with injuries or food that is too hot.
Someone with hypo-pain is at risk of not noticing when they are injured which can lead to further injury and may be at risk of self-injurious behaviour such as biting/hair pulling to feel a sense of pain regulation or a point of focus.
Pain is also our internal perception of bodily injuries such as toothache, stomach aches, headaches, and muscular-skeletal pains. Someone with hypo-pain may not have awareness if they have toothache and find it contributes to a sense of overwhelm without knowing why or that tooth decay isn’t treated in time risking abscesses.
Someone with hyper-pain may have vivid awareness of each bone and muscle in their body, and find it difficult to ignore aches, pains, and illness. Things like chest palpitations may feel overwhelming and create a sense of panic, or an overly sensitive desire to seek medical attention over less serious issues.
7.9. Interoception
Interoception is our awareness of different internal processes and regulations within the body. Some examples of this include noticing our body temperature e.g., awareness of dressing appropriately for the weather conditions outside, our sense of hunger or thirst, tiredness, hearing our heartbeats, pain (mentioned previously), and exhaustion.
Hyper-interoception might look like feeling the cold severely or overheating and becoming itchy when it’s hot, getting full very quickly or struggling with mood when you are hungry, a constantly parched throat, hearing your heartbeat, struggling with aerobic exercise due to sensitivity to muscle fatigue, or feeling a sense of tiredness easily.
Hypo-interoception might look like not noticing our medical needs as easily, not noticing when we are hungry or thirsty, overeating/drinking by not realising when we are full, pica (eating inedible things such as coins due to not noticing hunger), wearing too many layers in the summer or too few in the winter, overexerting ourselves in sports and risking injury, and not getting enough sleep or staying up late without noticing how tired we are.
7.10. Emotions
The Autism Research Group estimate that 50% of autistic people have alexithymia.
Alexithymia is the difficulty noticing, identifying, and regulating emotions in ourselves and others. It is a myth to assume that someone with alexithymia does not have feelings – they do, but they may struggle to identify them fluently or may use different language to convey feelings. This may mean that the person is dysregulated but struggles to realise that they are until they are overwhelmed and at risk of meltdown – when those feelings have become too pressing, or when only those strong feelings register. Leah Kuyper came up with the idea of Zones of Regulation to describe how regulated we feel into four colours:
- Blue zone (sad, bored, tired, sick).
- Green zone (happy, focused, calm, proud).
- Yellow zone (worried, frustrated, silly, excited).
- Red zone (angry, overjoyed, panicked, terrified).
The idea is to help a person realise what zone they are in to give them more control in order to self-soothe before they find themselves overwhelmed in the red zone.
There can be a belief that counselling is very focussed on feelings and you need to be ‘in touch’ with your feelings to attend, or that the therapist will interrogate you with the question “So how does that make you feel?”. My experience is that I am attentive to the feelings within what my clients say and may be expressive of what I think I am noticing so that those feelings can guide the meaning behind something, but feelings don’t need to be evoked and tend to spill up when they are ready.
We also need to recognise that communication involving stories, special interests, creative work, images, and snippets of a person’s history can be a rich descriptor of how they are feeling, expressed in a way that is unique to them. It’s more important that you feel regulated and accepted within therapy than that you use feeling words, and you shouldn’t have a sense of being pressured to be any way than what you are by a therapist.
8. Other Physical
8.1. Diet
We discussed how 90% of autistic people will have sensory processing disorder and each sense might affect diet; for example, with visual, there may be a preference for less vibrantly coloured foods like beige rather than multiple coloured mixed plates, with touch there may be preferences for hard foods or a revulsion against mushy food, with taste spices and seasonings may be overpowering, smell could cause the gag reflex at certain intense smells like boiled cabbage, and interoception may affect the sense of fullness or hunger.
Social imagination can create a preference for routine and structure which can make unpredictable foods (like fruit that changes taste as it ripens or between apples) distressing, or a desire for a routine dietary plan and distress if that plan is changed (“it’s Friday, where are the fish and chips?”). Social imagination can also create rituals and preferences in the preparation and making of food. When foods are changed, or new foods are introduced it can feel unpredictable and anxiety-invoking.
This combination can lead to ARFID, where a person’s diet is restricted quite severely and can lead to anxiety if a person cannot predict what food will be available (for example in a restaurant, or eating with friends). There can be a predictability, particularly with processed foods, but even then, a change in recipe or exception (bone in a chicken nugget) can ruin that food group. Having a restricted diet and preference towards processed food can also cause nutritional issues or weight issues.
A 2014 study stated that autistic children are four times more likely to have GI tract issues and have hyperinflammatory responses (a hypersensitive stomach) which can cause bloating, diarrhoea, acid reflux, and appetite issues. Interoceptive issues can make accurately knowing where and how the stomach hurts difficult, alongside social communication issues making the communication of this difficult with a GP. This can lead to a nasty combination of an unclear uncommunicated pain in the stomach from an overly sensitive GI tract.
Pica is the eating of inedible objects such as pennies – it can also develop as a way of meeting sensory needs such as a desire for hard foods, to try and ease stomach pain, or as a self-soothing strategy for anxiety. With Pica, we can ask ourselves what need the eating of these objects are meeting.
8.2. Allergies
There have been some associations between allergies and autism (see Spectrum News from 2018) linking higher rates of food allergies and sensitivities (including the previously mentioned GI tract sensitivities), skin allergies like eczema, respiratory allergies, and auto-immune or immune conditions. It is not clear if this is causal, but an autistic person may likely also suffer from more allergies.
8.3. Sleep
Interoceptive sensitivities may affect a person’s awareness of their tiredness. A person who prefers a visual learning style of learning may find screens appealing, but these can affect our circadian rhythm if used before bed.
Special interests and time perception can cause us to get carried away with a task and affect our nighttime routine. Sensory hypersensitivities can leave a person overstimulated which can make relaxing into sleep difficult, or mean awareness of things such as background noises or the weight of the blanket distracts from being able to relax enough to sleep. Social imagination may mean a preference for a fixed routine around bedtime, and distress if that is deviated from. GI tract issues or sensitivities to things such as noise may mean disturbance due to pain/cars on the road which can cause restless nights. All of this can lead to difficulties settling into sleep, and staying asleep through the night.
8.4. Processing time
All humans will process information at different paces and then respond to that information. If you are asked a question, there is usually a pause for you to answer. If you do not respond in time to the questioner or give a non-verbal placeholder to communicate what you are thinking (“ummmm”), they may try to explain their question/ask another question to stimulate you.
A lot is conveyed within a question on top of the sensory information within the environment that the person is trying to filter, and so some autistic people may appreciate extra time to respond. If they are not given a chance to process, space to reflect before communicating, or a bombarded with questions, they may become overwhelmed. If someone needs extra processing time, try leaving an extra five seconds longer than you normally might when you ask a question. Also, avoid asking several questions at once (something I realise I have done in some of the worksheet questions) to avoid confusion and give time for that question to be answered without confusion.
8.5. Learning styles
Edelson writes here about the four learning styles of visual (pictures, charts), reading and writing, auditory (hearing a teacher speak or having a conversation), or kinaesthetic (doing physically). He states that neurotypical children may have a preference for several learning styles, whereas autistic children may have more of a preference for one learning style. Many communication interventions seek to work with non-verbal/written learning through pictures (e.g. social stories) or action (e.g. Makaton sign language). Although not an autism-specific thing, it is useful to be aware of your preferences for learning styles so that you can be engaged with your learning and communication.
9. Behaviour
9.1. Masking
Masking is socially performed to hide traits associated with autism to fit in better in a neurotypical world. This could include things such as forcing yourself to maintain eye contact when it feels uncomfortable, pretending to ignore sensory information (e.g. not asking staff to turn down the music in a café), not stimming when you feel unregulated, resisting the urge to speak about a special interest, rehearsing social interactions, or using communication techniques such as active listening skills.
In Person-Centred theory, humans are a social species, and belonging is one of our most fundamental needs. Humans will do anything to earn that sense of belonging, including ignoring their own needs, and this can lead towards psychological disturbance where we lose contact with ourselves to ‘fit in’ – this results in incongruence and anxiety but at least we gain a sense of belonging rather than rejection or bullying. We learn how to perform and behave socially early in life, and this is especially true for an autistic person who learns to mask. Masking is adaptive and helpful in moderation, and we will all mask our true feelings/desires from time to time. However, with autism, there is more pressure to fit into a neurotypical world which can result in masking almost constantly socially and removing ourselves from our experience.
Masking is exhausting, as you are effectively performing (just like if you were giving a speech). Masking is also anxiety-provoking, wondering if you will be accepted or be able to continue masking. When we mask constantly, it can lead to clinical social anxiety in unknown situations as well as a sense of depression at the futility of not being fully known. If you are seeking therapy, one of the most healing things is finding a therapist where you can begin to unmask and have all parts of you accepted and understood. To find an environment where you can realise you are not disordered or wrong but can experiment with safely being.
9.2. Behaviours that Challenge
Behaviours that challenge (including meltdowns) are terms for when a person is overwhelmed and no longer in control. The person who is overwhelmed is incredibly anxious and distressed and trying their best to control the environment to feel regulated. The behaviour itself can appear ‘naughty’ or ‘unsafe’, but we need to understand that the person is just trying to calm the environment to the best of their ability rather than trying to make a scene or be challenging. Some examples of BtC include self-injurious behaviours such as headbanging/biting oneself, running away, shouting, hitting/biting others, destroying property, as well as demand avoidance.
United Response (2015) wrote an excellent paper on positive behavioural support planning to help a person who is at risk of showing BtC. It considers all behaviour a form of communication including BtC, and considers firstly how we can recognise the need the BtC is meeting, secondly how we can implement strategies to reduce the likelihood of a person becoming overwhelmed, and thirdly how we can reward and encourage positive behaviour (punishing negative behaviour does not work – see my spoof article on if torture would rehabilitate.
We mentioned how 90% of autistic individuals have sensory processing sensitivities. BtC is often caused by sensory overload where there is too much sensory information for the person to self-soothe and regulate so they become overwhelmed and at risk to themselves or others, for example, a room feels too noisy with a loud TV on, so they smash it. Learning a person’s sensory profile can help to understand what might pose a risk for sensory overload and with that a risk of BtC.
The sensory overload may be because of the environment (e.g. noise, light, smells) but it may also be internal to the person (e.g. head banging may be caused by toothache). A person may also find that the Triad impacts BtC, for example, social interaction could become too intense and overwhelming or masking too exhausting to continue. With social imagination, it may be that changes in routine or unpredictable environments create too big a sense of chaos in the world and a person is dysregulated and anxious.
Proactive strategies seek to create environments where a person can be regulated (e.g. low-sensory environments), in control, and able to communicate distress. A proactive strategy would look at previous BtC, looking at exactly what happened, what/whom it was in response to, and the consequence of that behaviour (e.g., ‘It was my time to present so I shouted and swore which meant I got sent out of the classroom and did not have to present’). Proactive strategies seek to avoid what/whoever caused the overstimulation and teach other less challenging ways of getting their needs met (could they, for example, say that they do not want to present today or have not prepared?) and an understanding of why the alternative might be more advantageous.
Reactive strategies again consider the person’s unique sensory profile and how their ASC is expressed. From that, and specific examples of BtC, it looks to regulate the person. An example might be removing the sensory stimuli for someone who is hypersensitive (e.g., quiet the room down, or turn down the lights), vacating the room to give the person a chance to be alone, asking the person to go on a walk outside of the environment, or if it is triggered by a specific person that person distancing themselves.
Reactive strategies might also seek to reduce harm done to the person or others around them for example putting a cushion in the way if a person is head-banging on a wall or removing a sharp object from the room if it is safe to do so. Restraint is sometimes used if a person is at risk of harm to themselves or others – this should be an absolute last resort and not done by a person without training, it should also only be done if it meets the person’s care plan (e.g. if you have hyper-touch and someone intrusively restrains you it can be incredibly traumatic). Restraint generally can be quite shaming and distressing for the person being restrained. In the short term restraint might reduce harm, but in the long term contributes to BtC rather than reducing it.
10. Mental Health, Support, and Counselling.
Our mental health and well-being are an interchange between our biology and our environment. The world is designed for neurotypical people in terms of access and communication, and people who are neurodiverse face many barriers, misunderstandings, and even discrimination. This can lead to an increase in mental health needs.
10.1. Mental Health
It is estimated that 25% of the general population will have a mental health problem during their lifetime; however, for autistic people, this figure is more like 70-80%.
10.1.1. Anxiety
Anxiety is a large spectrum of diagnosable mental health issues. It can present quite differently between people in their thoughts, within the body or emotionally, and be triggered uniquely for everyone. The NHS calls anxiety “a feeling of unease, such as worry or fear, that can be mild or severe” and includes panic disorders, phobias, social anxiety, generalised anxiety, and post-traumatic stress.
Autism is characterised by social communication and social interaction difficulties, so it is unsurprising that rates of social anxiety are high. The Autism Research Group cite how neurotypical social anxiety is often about embarrassment from others whereas social anxiety in autism is more linked to performance. Namely, a person cannot rely on self-soothing techniques such as stimming as freely in social settings, and a sense of having to perform or not knowing how to respond socially. An autistic person may have a perpetual sense of getting it wrong and feel an intolerance towards the uncertainty of how a social interaction is going.
10.1.2. Obsessive Compulsive Disorder (OCD)
Linked to anxiety, autism is also marked with social imagination needs where routine and structure are important and losing that routine can be incredibly distressing. OCD is another neurodiversity that has some overlaps with ASC. A person with OCD will notice a thought that demands they do something, then a compulsion to do that thing, and intense anxiety and dread until it is accomplished. A person may have both ASC and OCD and the two have overlap around routines and rituals that need to happen for the person to feel secure.
A person with ASC will face similar anxiety if their routine is broken, which may seem disproportionate to the change, but we need to remember that routine and structure provide certainty in a chaotic world. This could include changes to rituals such as bedtime routine, settings where we cannot predict outcomes as easily, not being able to stim to self-soothe, or if there is an interruption to a special interest.
10.1.3. Grief
Being a parent to an autistic child involves the beauty of learning about their unique ways of being (hence writing this article as everyone with ASC has their own unique profile). The connection and attachment can be very powerful, and when someone dies there can be an added layer of loss of losing someone who understands and accepts them. We also talked about the importance of structure, routine, and safety in a chaotic world, and losing a loved one represents the ultimate loss of that. Around the time of the death, there is likely to be a lot of change – perhaps a moving of home, a change of role within the household, a lot of administration around the death.
Funerals can also be very social neurotypical ritualised events that can be confusing with expectations of ‘the right way to grieve’ when everyone’s grief is unique and at their own pace. When someone dies, we can also use vague language e.g. “They’ve passed away”, “They’re looking down on us”, or “They’re in the clouds with the angels” which can be confusing if taken literally when one of the tasks of grief Worden mentions is emotionally locating that the person has really died. Grief can also evoke powerful feelings in us such as anger, and intense pangs of grief; if we have alexithymia, these strong feelings can be even harder to recognise or manage.
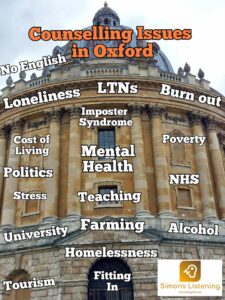
10.1.4. Loneliness
Autistic people may struggle socially or feel socially anxious, but they still have a need for connection. A combination of wanting close connections and friends or wanting to fit in and belong in a group, alongside feeling different or unable to connect/understand social etiquette can be very isolating and lonely. There can be loneliness when trying to connect with people between the type of authentic connection they may enjoy versus the models of friendship they encounter, e.g. with their special interests. We can then feel lonely when we do have not enough connections, but also when the connections we have aren’t meeting our relational needs.
A number of charities set up groups for autistic people; if you’re based in Oxford you might appreciate these links on Oxford Aspie’s site. It can also be useful to see if there are groups, gatherings, and events for people with similar special interests e.g. using Meetup. The internet, online groups, and gaming have been useful in providing some connection over a shared interest and can contribute to meeting some of those social needs. Virtual meetings or text-based communication also give us more time to process, respond and have a sense of control over what we discuss (e.g. in forums). However, we need to consider internet safety and the risks around exploitation from others.
There can also be cultural NT extrovert expectations that spending too much time alone means that a person is lonely. Autists often have far greater tolerance to isolation than NT people. They can also derive great joy from special interests and hobbies and have less of a need for a NT or extroverted level of social interaction. Questions like “You must be lonely” can cause a person who is quite self-sufficient to again question if they are getting it right or push themselves into uncomfortable social interactions.
10.1.5. Trauma
Trauma is a human response to a situation that is overwhelming, frightening, or existentially disturbing. It is not a weakness, but the body’s way of coping and processing. Sometimes traumatic information can lead us to keep reliving the situation and find ourselves disturbed longer term by an event (e.g. developing PTSD if we were a victim in a crime) or continual series of events (e.g. developing CPTSD if our caregiver abused us continually or we perceived them as doing so). Trauma isn’t guaranteed from an event or series of events (otherwise ambulance drivers or police officers would be perpetually traumatised from their work), but more concerns how the traumatic event(s) impacted and are interpreted by us emotionally and existentially – i.e. it’s our perception more than the event.
An autistic person may find an environment traumatic and overwhelming, that a NT would not – for example continual sensory overload from noise, places where you feel wrong/misunderstood/bullied, sudden changes in schedules that feel chaotic and out of control (control being a protective factor against trauma). Dr Freya Rumble wrote more on autism and PTSD where she cites that rates of PTSD could be up to ten times higher in autistic people than NTs. Because of the prevalence of trauma and perpetual sense of feeling different, as well as interoceptive issues/alexithymia, an autist may also need help to recognise when they are experiencing trauma, whereas an NT who has experienced a traumatic event and suddenly starts experiencing palpitations, flashbacks, sweats and a sense of dread or terror may be more inclined to feel something is wrong and seek support.
10.1.6. Suicide
Suicidal thoughts are more common than people think and talking to others can reduce, normalise, and soothe them. If you are having suicidal thoughts, and especially if this is leading towards ideation or a plan, please call Samaritans for free on 116 123 or you can email [email protected]. It is worth exploring what the suicidal thoughts are about: perhaps you are ruminating on the act of suicide or are disturbed by thoughts of this, maybe it’s about escaping from a situation or some respite from life, or maybe it’s about being noticed or missed? Suicide can be a scary thought to hold in our heads and sharing it with a professional or supportive other can help to make sense of it and keep you safe.
Some risk factors associated with suicide are likely to be higher in autism: having a mental health condition, other neurodiversities, feeling isolated or not belonging, not being able to communicate out distress or feeling adequately heard, difficulty in identifying feelings (alexithymia), trauma or overwhelm from situations, socioeconomic disadvantage, losses & bereavements, or chronic pain.
10.1.7. Self-harm
Self-injurious behaviours can include more than just cutting, for example: substance abuse, head banging, pica, reckless behaviour, binge eating/purging etc. Instead, we can view self-harm as a coping strategy and may want to consider how all behaviour that helps us cope or rewards us could become self-injurious or neglectful if done to excess (for example, if I play too many video games I won’t get enough sleep and may neglect to eat/work/exercise; if I shop or gamble too much I may find that I have no money). Cutting specifically may relate to suicidal ideation, but more often it is a coping strategy. When someone uses self-injurious behaviour, we first want to ask ourselves what need the behaviour is meeting. Is it helping to cope with strong emotions, providing a sense of control, communicating distress, punishing themselves, or maybe it’s about feeling alive?
Once we know what need the behaviour is meeting, we can look to see how else that need can be met and reduce the harm e.g. could we put ice on the skin or use a red biro rather than cutting, chewing on hard nuts or chew toys instead of pica, or could we use a cushion if we headbang? You may find this guide from the University of Oxford helpful or Carrie McColl’s article if you have a child who self-harms; charities like Harmless also specialise in this area.
With ASC there are some added risk factors or communication needs that self-harm might meet. Consider sensory processing needs; a person who is hypo touch/proprioceptive/vestibular may find things like stomping/head banging/punching/fighting/rough play help them to feel regulated and create an awareness of their body and its position in space. If a person is overwhelmed by sensory issues, self-harm may provide a point of single focus or to cope with the overwhelm. A person may also find pica enjoyable if they have preferences for hard food (e.g. eat pennies). Self-injurious behaviour may also be used to cope with pain (e.g. have you ever ground your teeth when you have a toothache?) that cannot be communicated due to communication issues or sensed due to interoceptive sensory issues.
Self-harm can also be linked to stimming behaviour (e.g. hair pulling [trichotillomania] is a common stim but if done excessively when overwhelmed could be self-injurious). With social-imagination self-harm can create ritualised behaviour, e.g. around cutting and cleaning the wound after that can create a sense of control in a chaotic world. Autistic people are also more likely to be bullied, or culturally isolated, and can struggle to communicate this in a way to provide relief which can be a risk factor for self-harm.
10.2. Abuse
10.2.1. Bullying
Bullying is the repetitive and targeted hurting of another person or group of people. It isn’t always obvious or overt and may include neglecting social exclusions and sarcasm or making jokes at an autist’s expense. An autist may not even be able to read that they are being bullied due to honesty in communication and trust which could add to the dangers of it. It mirrors abuse in that it can be emotional, physical, sexual, financial, psychological, and institutional by not being accessible. Ambitious about Autism reports that 75% of autistic people have reported bullying and only 50% feel safe in school, but bullying and abuse are not just limited to school, we can face bullying in our social groups, online, and in the workplace as adults.
Autism meets the criteria for disability within the Protected Characteristics of the Equality Act 2010. This means that workplaces, schools, hospitals etc should make reasonable adjustments to promote autistic inclusion. What I am saying is that bullying and being institutionally excluded are not okay under the law. Bullying is usually targeted at people who are seen as different or in some way less able to defend themselves. With autism, communication and social interactional needs are likely to make the person more vulnerable to bullying/abuse and less able to recover from that abuse within a secure friendship base. Repetitive behaviour like stimming or sensory overwhelm are also likely to make an autistic person stand out in social environments and risk bullying.
If a person with ASC is distressed and uses behaviours that challenge, that can be seen superficially as ‘bad’ or difficult, which can create labels and misunderstandings. Finally, there are still prevalent misunderstandings, discrimination, and labelling of autistic people that can cause bullying. An autistic person may be hyper-vigilant towards incidents of bullying and in a perpetual state of uncertainty on whether their communication is acceptable to a group or if they are about to be bullied. When they are bullied, they may struggle to voice or report it and doubt whether it is normal behaviour or banter/jokes. For more information on bullying and autism, you may find this link from Anti-bullying Alliance helpful.
10.2.2. Exploitation & abuse
Exploitation, abuse, and neglect are more extreme forms of bullying and can lead to a need for police or safeguarding involvement to protect the person. Abuse can be discriminatory, sexual, physical, financial/material, domestic, neglect through omission, self-neglect, modern slavery, cultural, and organisational. Abuse is targeted at an individual, and to constitute abuse that individual needs to be unable to prevent the abuse. Autistic people are vulnerable to abuse due to the same reasons identified within the previous section, but there are some added vulnerabilities to not having the capacity to stop the abuse.
Having a learning difficulty can prevent us from knowing if we are being abused, social vulnerabilities such as being honest in your communication and not being as aware when others are being dishonest can lead us to not know if we are being exploited; social vulnerabilities and loneliness can make us want to belong and leave us vulnerable to gangs/terrorism/financial abuse, and social interactional issues may mean that we struggle to reach out to a trusted person to get help when we are being abused. If you are the victim of abuse, neglect, or exploitation you may find some of the links in the Preventing Exploitation Toolkit helpful; if you are in immediate danger you can contact the police on 999 or 101 for non-emergency, and your local county council will have its own child and adult safeguarding teams.
10.3. Support
Support can come in different ways from informal, carers, local authority, charities, and private support. Our immediate support will typically be the people closest to us; our family, carers, partner, or those we live with. Likewise, the people close to us are unique with their own needs for understanding, rest, and support. Just as there can be a sense of not belonging in social environments like schools, we can also feel misunderstood, or our needs and expectations not met within our family unit.
The local authority and other public services may also support us. Things like the autism team, an “Education, Health, and Care Plan” (EHCP) at school, support or care workers if we have had a care assessment, social workers if there have been safeguarding concerns, or from the NHS such as our GP/nutritionist/physiotherapy, and the benefit system.
Finally, there may be a gap between what is publicly available, and the support that charities or private organisations provide. This could include respite organisations (e.g. the Newman’s Holiday Trust to take children away over the summer), counselling, social groups, private physio or sensory work, work/education/training opportunities, and budgeting support. For Oxford, The Mind Guide provides an excellent list of local and national charities and organisations that work with a variety of our needs.
10.4. Therapy
Autism is not something that we can cure – it’s a neurodiversity – nor is there a medication to change some aspects that can be a struggle. What I am trying to say is that autism isn’t a defect that needs treatment, however, all the different things mentioned in this checklist can present multiple issues that can be useful to unpack within therapy.
Therapy (counselling) can help us by:
- Increasing awareness of our feelings in the way they uniquely present to us, managing when they are too intense, or how our needs lead us to behave in ways that we would like to change.
- Treatment of coexisting mental health conditions can often be unique in the way they present and are affected because of ASC.
- Processing bullying, trauma, and social exclusion.
- Coming to terms with a diagnosis (whether self-diagnosed or medically).
- Coping with changes, aspirations, and losses.
When you seek therapy, you may want to consider some factors:
- Does your therapist have autism, or are they aware of the experience of an autistic person?
- Are your communication preferences accommodated? Do you need to make eye contact? How is stimming promoted within the therapy room? Can you get up/pause/move/adapt the space to meet your sensory needs? Would you prefer to work remotely through video messenger or phone?
- How much does the therapist direct the sessions? Some modalities (such as my own as a person-centred counsellor) are very open which can be hugely beneficial for tolerating uncertainty of direction and give you a lot of control, however for some people that can be quite overwhelming and agreeing on a clear direction for the therapy or having worksheets/homework/programs can provide a sense of structure.
- Will it be psychoeducational, group programs, or one-to-one?
- Will you be able to incorporate your special interest within the work?
- Can you and your therapist review regularly to check if it is meeting your needs?
My hope in writing this, and in you considering the questions within the questionnaire is that you can better understand the uniqueness of how your autism affects you, and gain the language to better describe your autism to professionals and others in your life to create a more inclusive affirming world around you. If you would like to consider counselling for any of the issues raised within this article, please feel free to check out my profile and get in touch.
Special thanks to Sophie’s Proof Reading for copy editing, and Cat Abrams & Zak Martell for their feedback
Simon is a Person-Centred Counsellor working remotely or face to face in Oxford. He offers a relational approach to counselling at your pace and respecting your unique way of processing, communicating, and experiencing the world. Feel free to follow me and get in contact if you would like to work together.
077 498 70502
[email protected]